Research Insights
How Much Diagnostic Imaging Is Inappropriate and What Does It Cost?
Why This Study Is Important
Overall utilization of diagnostic imaging procedures has been increasing rapidly in the U.S., and we now spend well over $100 billion on these procedures each year. At the same time, evidence is mounting that a nontrivial portion of this care is provided inappropriately, conferring little value to patients and perhaps causing harm. This study expands that evidence base by examining the extent of inappropriate diagnostic imaging for three common conditions within a large group of commercially insured adults in Massachusetts.
What This Study Found
- For all three conditions, the percent of X-rays and MRIs provided within 30 days of the initial visit increased between 2010 and 2013.
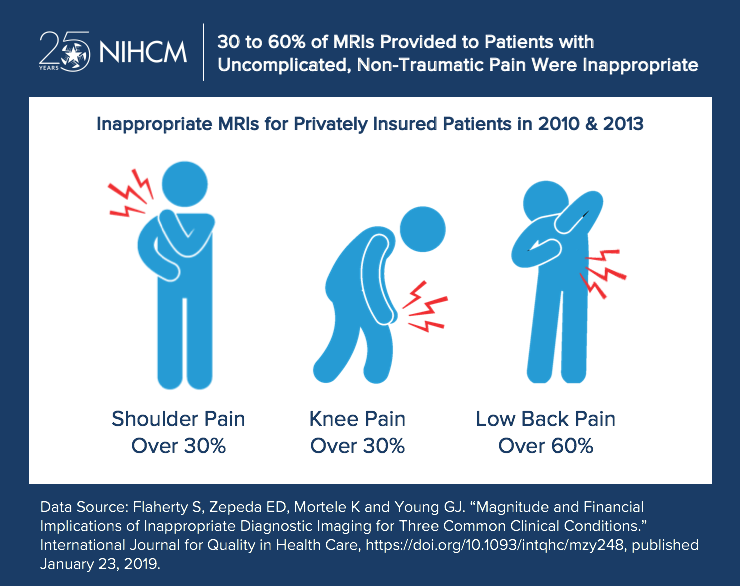
- More than 60 percent of lumbar spine MRIs and approximately 40 percent of lumbar spine X-rays received in the 30 days after the visit were deemed inappropriate in both 2010 and 2013. For knee and shoulder pain, more than 30 percent of the MRIs were inappropriate in both years. Similar results were obtained using a 60-day window.
- Compared to patients for whom MRI imaging was appropriate, patients receiving inappropriate MRIs were significantly less likely to undergo surgery for their condition within 90 days, suggesting that there was less clinical urgency for these latter patients.
- Using spending data only from the Massachusetts study population, inappropriate imaging for the three conditions was conservatively estimated to have cost commercial insurers from $4.6 to 5.5 million in the two study years. Inappropriate imaging costs would be much higher if computed nationally across all imaging modalities and clinical conditions and if patient cost sharing were considered.
What These Findings Mean
A number of factors may be related to the inappropriate use of diagnostic imaging procedures, including low awareness or use of ACR guidelines among providers, patient beliefs that all imaging is beneficial, defensive medicine, high levels of imaging capacity and financial incentives facing providers. Initiatives that may address some of these factors include pre-authorization requirements, efforts to improve knowledge and uptake of appropriateness guidelines, and incenting patients to be more judicious consumers by increasing their cost sharing. More research is needed to understand the drivers of inappropriate imaging as well as the extent to which proposed solutions will be able to trim inappropriate use.
More About This Study
This study used commercial claims data from Massachusetts to assess the appropriateness of MRIs and X-rays provided to healthy adult patients first presenting with uncomplicated low back pain or non-traumatic knee or shoulder pain. Inappropriateness of diagnostic imaging received within 30 and 60 days of the visit was determined by whether or not the care adhered to the imaging guidelines of the American College of Radiology (ACR). The researchers also assessed how frequently patients with MRIs underwent surgery within 90 days. Chi-squared tests were used to compare rates of inappropriate imaging over time and whether follow-up surgery rates differed by whether the MRI was appropriate or not. Costs of inappropriate care were computed net of the costs of care that would have been appropriate.
Flaherty S, Zepeda ED, Mortele K and Young GJ. “Magnitude and Financial Implications of Inappropriate Diagnostic Imaging for Three Common Clinical Conditions.” International Journal for Quality in Health Care, https://doi.org/10.1093/intqhc/mzy248, published January 23, 2019.
More Related Content
See More on: Cost & Quality

