Webinar
Homelessness & COVID-19: A Merger of Two Epidemics
Time & Location
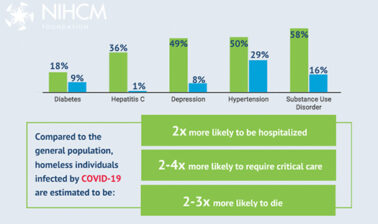
The COVID-19 pandemic has placed a spotlight on the homeless and home insecure population, highlighting the existing health challenges faced by this community and the additional risks posed by COVID-19. A new analysis estimates that homeless individuals infected by COVID-19 are two to four times as likely to require critical care and two to three times as likely to die compared to the general population. This webinar looked at the state of homelessness in the US and its critical impact on health and provided strategies to improve outcomes for homeless individuals both in the short and long term.
Speakers discussed:
- The complex relationship between homelessness and health and how health centers and other organizations are responding to improve care, increase housing access and ultimately eliminate homelessness
- The impact of homelessness on youth and how health plans and community partners are working to increase access to clinical care and services
- An organization's efforts to meet the needs of homeless LGBTQ youth by offering free training and resources and ensuring critical funding and services for all youth
Cait Ellis (00:00:00):
Good afternoon. I'm Cait Ellis, Program Manager at the National Institute for Health Care Management Foundation. On behalf of NIHCM, we want to extend our thanks to healthcare, frontline, and essential workers for keeping us safe during COVID-19. This is a challenging time and now more than ever we must work towards a healthy, equitable, and just future for all. Our goal today is to share information on the relationship between homelessness and health and shed light on how different communities face increased risks and challenges, including racial minority groups, youth, and the LGBTQ community. We will also focus on solutions and evidence-based strategies to improve the health and wellbeing of individuals experiencing homelessness during COVID-19 and in the long-term.
Cait Ellis (00:00:47):
The relationship between homelessness and health is complex and bi-directional. Poor health can contribute to poverty, housing insecurity, and ultimately homelessness as experiencing homelessness can worsen existing health problems, cause new ones, and make treating all conditions challenging. COVID-19 has only exacerbated these challenges. A recent analysis estimates that homeless individuals infected by COVID-19 are two to four times as likely to require critical care, and two to three times as likely to die compared to the general population. To explore short and long-term strategies to address all of these challenges, we are pleased to have a prestigious panel of experts with us today.
Cait Ellis (00:01:30):
Before we hear from them, I would like to thank NIHCM's, president and CEO, Nancy Chockley, and the NIHCM team who helped to convene this event. You can find biographical information for all of our speakers on our website, along with today's agenda and copies of slides. We also invite you to live tweet during the webinar using the hashtag, homeless health.
Cait Ellis (00:01:50):
I am now pleased to introduce our first speaker, Bobby Watts, CEO of the National Health Care for the Homeless Council. Bobby has more than 25 years of experience implementing homeless health services. His extensive and diverse background gives him a unique perspective on the intersection of homelessness and health and the impact of COVID-19 on this population. We are so grateful he is with us today to share his insights, Bobby.
Bobby Watts (00:02:17):
Hello, thank you very much, Caitlin. I am honored to be here and I am really honored to be here in front of all of the participants. Thank you for your time, and I'm thrilled that we were able to focus on this important topic of looking at the impact of health on people experiencing homelessness and, as you mentioned, that it's bi-directional. I just want to, first, just share an overview, an outline, of what I'll be talking about in the next 10 to 12 minutes. I want to explain who the council is and the work that we and the Health Care for the Homeless programs and medical respite programs do, and why it's relevant to you, those who are involved with NIHCM. I also want to give a very brief overview of homelessness and health care, and just want to focus on one of the innovation foci of medical respite care, also known as recuperative care in California and a few other states. Then I want to talk about the response to and lessons from the COVID pandemic as it affects those people who are experiencing homelessness and those who are providing services to them.
Bobby Watts (00:03:32):
First, just to talk a little bit about who the National Health Care for the Homeless Council is and why we exist, and we have a brand new mission statement as a result of a strategic planning process. Just want to read that to you because it's so important, and hopefully it describes who we are, what we do, and why we are doing it. It reads, "Grounded in human rights and social justice, the National Health Care for the Homeless Council mission is to be build a high quality equitable healthcare system through training, research, and advocacy in the movement to end homelessness." Just a few parts there. We really are focused on equity as well as quality. In fact, our last conference, which unfortunately had to be canceled as many were, but we're going to keep the thing for next year, is that equality equals quality plus equity. It should be, equity plus quality. You can't have real quality healthcare if equity is not at the center of what you do.
Bobby Watts (00:04:34):
Secondly, a big part is that we are committed to working to end homelessness, and we know that is through direct services but also it is very important that we do that through systemic changes, policy changes at the federal and local levels. Just a word about who we are. We are a network of Health Care for the Homeless programs, and I'll talk a little bit more about that, but we also have our network of individuals. We have three main network constituent bodies. We have about 2,000 clinicians in our clinicians network. These are people working in clinics, working in programs with hands-on clinical care that they deliver to people experiencing homelessness. I'll point out, I'm using the phrase, people experiencing homelessness instead of homeless people throughout, because we really want to emphasize that homelessness does not define a whole person's existence, it does not define who they are.
Bobby Watts (00:05:41):
It is an experience that hopefully will be short-term and hopefully will end, but it is an experience versus an innate characteristic of the person. We have 1500 members in what we call our national consumer advisory board. Consumers are those that are patients in our programs. We really understand if we are going to get better at anything that we do, that we have to listen to those that we are serving. We have to listen to our customers. That's the first rule of business. Unfortunately, healthcare does a fairly poor job of that as does most homeless services. We want to make sure that we are listening to those that we are serving and also to help our program, members of our organization, our members, also make sure that they have the systems and processes in place to listen to those with the lived experience of homelessness.
Bobby Watts (00:06:48):
Finally, we have about over 1500 members of our respite care providers network. Again, these are people in the frontline working in medical respite programs, and I'll share a little bit about that in a minute. There are 300 Health Care for the Homeless programs across the country. There is at least one in every state. What these are, these are federally qualified health centers. There are about 1400 federally qualified health centers, and 300 of them have a program specifically to make sure they know how and with a focus on delivering care to people experiencing homelessness. Their section under the Federal Health Center program is called section 330(h), or also just known as HCH or Health Care for the Homeless program.
Bobby Watts (00:07:45):
I mentioned, in 2018, over one million people experiencing homelessness were seen in these programs. I mentioned that 250,000 were seen in California. In many ways, California is the epicenter of much of homelessness in the country, and certainly of unsheltered homelessness. Like all federally qualified health programs, health centers, they meet all of the conditions, all of the requirements, providing primary care, mental health services, dental services, outreach prevention. In addition, there are two other requirements that Health Care for the Homeless programs have to meet that other federally qualified health centers don't have to, and that is, they have to do outreach in some way. It's realized that people experiencing homelessness have been estranged from the large stream main health system. We need to go an extra step in outreach in some way to reach out to them. They have to provide, or have an extremely strong linkage to mental health services and substance abuse services or substance use disorder services, together known as behavioral health.
Bobby Watts (00:09:04):
I'll just say a few words and you'll have the slide, so I won't read all of this, but the integrated health has been a part and parcel of the Health Care for the Homeless movement for 35 years. From the very beginning, we said, "We have to treat the whole person, we have to treat social determinants of health, we have to integrate behavioral health and primary care, and we have to use trauma-informed care and harm reduction practices." We've been doing that sometimes even before those were the terms that have come into use, but the principles and the practices were there. In some ways, I like to say that the larger health system is catching up to the Health Care for the Homeless movement. Just one picture of how focused we are at integrated behavioral health, the last stat there is that 4% of FQHC patients are found in the 300 Health Care for the Homeless programs, but those 300 programs delivered 38% of all medication-assisted treatment services, which is really important for addressing the opioid epidemic, which has not abated in the time of COVID.
Bobby Watts (00:10:23):
Caitlin already addressed the interrelationship between homelessness and health, and I just want to emphasize that for every health condition it is found at elevated prevalence rates, among people experiencing homelessness compared to the housed population. We see this most, we see the poor health and the lack of access to healthcare and the difficulty of treating someone when they don't have a home, in this statistic. That on average, people without homes, especially those on the street, die at an average age of 50, compared to an average age of around 80 in the general population in the US. 30 years of life is lost largely as a result of not having safe and stable housing, one of the most important social determinants of health.
Bobby Watts (00:11:26):
I'll just summarize this current slide that the health needs and utilization of people experiencing homelessness are up. They use emergency rooms, hospitalization or hospital stays, use EMT calls, unfortunately, engaged with the police, you get sent to jail at higher rates. Their social needs are higher, but failure to meet those needs leads to barriers to healthcare access. What we have to do in the Health Care for the Homeless program and what we have to do as a healthcare system, and as a society, if we are going to promote equity, is to make sure that we remove the barriers so that people can get care. There is a phrase we use in healthcare or in social services that some clients are service-resistant. I really think it is that our services are client-resistant. They're not adapted to the needs of that person, and that is what we try to do in Health Care for the Homeless and what we need to do as a country.
Bobby Watts (00:12:40):
The next few things I just want to talk about his medical respite. I say, this is an innovation. It really has been around for 30 years, 35 years, but people are just really beginning to focus on it. What medical respite is is a service or facility for people without homes who no longer have a clinical need to stay in the hospital, but they don't have a safe discharge option. Without this discharge, without medical respite, they end up being discharged back to a shelter that's not really equipped to handle them, to a friend's couch, or sometimes even to the street with the predicted outcome that their health deteriorates. They end up back in the emergency room, back in the hospitalization at huge cost to them personally, in terms of poor health, but also at a huge cost to the healthcare system.
Bobby Watts (00:13:37):
What medical respite does is provides that place. There are about 100 programs across the country. One of our strategic priorities is we want to expand right medical respite. There have been some studies, and the citations are in the slide, just showing that they reduce hospital stays, they reduce the cost, they also reduce the rate of readmission, and they also reduce the ED visits. When medical respite works best, it is a gateway to permanent housing, usually permanent supportive housing, but it always will make sure someone is linked in with case management so that their medical needs are met and they are linked to primary care and then can break the cycle of poor health and high cost which helps no one, it doesn't help the healthcare system, it doesn't help the shelter system, it doesn't help anyone.
Bobby Watts (00:14:38):
Caitlin mentioned that people who are experiencing homelessness are at increased risk from COVID. Part of that is because they are generally in either congregate settings or they are not able to practice social distancing. Fortunately, the council was involved with both giving guidance or giving advice to CDC and HUD, some of which they incorporated into their guidances to states and cities on ways to protect people experiencing homelessness and also to reduce transmissions, both in congregate settings and in unsheltered settings, such as those living on the streets, those living in encampments. What every community had just determined was how would they provide isolation and quarantine for people without homes? What many of them did set up was alternative care sites, sometimes renting hotel rooms, sometimes setting up part of a convention center that they turned into a healthcare facility. What really that was, we realized that really is medical respite or meeting the needs of the goal of medical respite to meet the healthcare needs of people without homes.
Bobby Watts (00:15:57):
That has really increased the attention on medical respite, and we're thrilled about that. We're glad that the CDC recommended more humane treatments for people in encampments, provide more street medicine, more doctors and nurses and outreach teams going there. Providing handwashing stations. The number one CDC guidance for reducing transmission was to wash your hands for 20 seconds. If you're living in an encampment on the streets, you don't, some cities have put in handwashing stations, they've put in toileting facilities there.
Bobby Watts (00:16:36):
My last thing which I will say is that the pandemic has brought into sharp relief the inequities and inadequacies of our health and social systems. We see the effects of systemic racism and how the burden of COVID is borne by people, especially African Americans and Native American Indians, but also in some places, Latinx and, and also Asians in some places. We also see the effect of not having a system that regard or systems that regard healthcare and housing as human rights. The virus does not recognize state lines, but whether you live in one state or another, and based upon whether they have expanded Medicaid or not, will largely determine what kind of care you can get. We see that in COVID. We see that for substance abuse, substance use disorders, we see that across the board. We have to improve as a nation and the council has really placed equity at the core of our work in promoting quality services by our members and advocating for humane and just services in this country.
Bobby Watts (00:17:57):
I will close with saying, we have a wealth of resources on our website which, I believe they will be made available to you. A lot about COVID, some about our work around anti-racism in order to reduce race inequities in this country, and also some about medical respite. I really thank you for your time, and I look forward to your questions and my fellow panelists and the ensuing discussion. Thank you.
Cait Ellis (00:18:33):
Thank you, Bobby, for helping all of us understand more about homelessness and the types of solutions, both short and long-term, that could really make an impact for these individuals and families, and for highlighting the importance of focusing on equity and quality in addressing these challenges. Under the leadership of CEO, Dan Hilferty, Independence Blue Cross is committed to improving the health and wellbeing of youth and young people experiencing homelessness. To hear more about these efforts, we are now joined by Reverend Dr. Lorina Marshall-Blake, President of the Independence Blue Cross Foundation and Vice President of Community Affairs at Independence Blue Cross. We welcome her to the panel to share more about their efforts in the community and how they are addressing the health challenges stemming from homelessness and COVID-19. Lorina.
Dr. Lorina Marshall-Blake (00:19:19):
Okay. Thank you so much, Caitlin. Again, good afternoon to everyone. Again, I'm going to thank the National Institute for Health Care Management Foundation for inviting me as a panelist on this webinar. Again, my fellow panelists, I greet you. Bobby, I've learned so much. Every time I think I know something, I learn an additional amount, so thank you for your informative presentation. Then I will also be remiss, I know there are many Blue Cross plans that are along with us, so again, I want to recognize our fellow Blue plans joining from across the country. Again, [inaudible 00:19:58] Lorina Marshall-Blake and I consider it a privilege. Just as I heard Bobby speaking today, the work that I do is work of passion and love, and serving as the President of the Independence Blue Cross Foundation. I also have another title, which is Vice President of Community Affairs for Independence Blue Cross.
Dr. Lorina Marshall-Blake (00:20:19):
But let me tell you a little bit about the foundation. Again, when we look at collaboration and we look at connection, how do we bring, even as I listened to Bobby, how we bring these different environments together so that they collaborate and they all work together. The foundation is the private charitable corporate foundation of Independence Blue Cross. It was founded with the mission to lead sustainable solutions. I emphasize sustainable solutions to improve the health and wellbeing of the communities we serve. Again, it's not about Independence, it's all about the community. I always say we're boots on the ground. We believe in leveraging cross-sector collaboration, so it's not just us, it's others at the table with us to address the greatest health challenges facing our community. I think it goes without saying that we have many challenges today and none of us, I think you may join me, can address them lone without working together. But you know who can address them, all of us together. That's why I'm excited about being a part of this panel.
Dr. Lorina Marshall-Blake (00:21:30):
Again, the key is through collaboration and connection. I'm excited to talk about how we're working with and supporting community [inaudible 00:21:38] organizations who are creating change in healthcare for our most vulnerable population. Again, it's not about us, but it's about all the other people that we are indeed working with. The foundation, what we do, we award grants to communitybased nonprofits, privately funded health centers, and accredited nursing programs in Southeastern Pennsylvania, which includes Bucks, Chester, Delaware, Montgomery, and Philadelphia counties. What we focus on, again, is an access to care, the healthcare workforce, innovation in the nonprofit sector, and national health issues. I think, again, it goes without saying that COVID-19 and homelessness are major healthcare issues.
Dr. Lorina Marshall-Blake (00:22:26):
To date, the foundation has awarded more than 40 million in grants to more than 200 partners reaching nearly 300,000 residents in Southeastern PA. Investing in the education and professional development of nurses is one of the foundation's top priorities. I think with this COVID-19, we have seen how vital nurses have been to this whole pandemic and epidemic, and being on the front line. Again, when I think of nurses, they're compassionate, they're caring, they're lenses. They bring their skillset, but they also bring compassion with it. Through our Nurses for Tomorrow program, we partner with national nursing organizations, nurse leaders, and regional nursing schools to prepare the next generation and [inaudible 00:23:12] looking forward to the next generation of healthcare heroes through grantmaking and leadership opportunities.
Dr. Lorina Marshall-Blake (00:23:20):
Under the umbrella of Nurses for Tomorrow, our nursing internship program, and I'm delighted to say that, even with the pandemic and even with COVID-19, I have 30 nursing interns that are working with me this summer. The program is designed precisely for undergraduate nursing students who seek to understand nontraditional roles in nursing. Through our Blue Safety Net program, we fund nearly 50 community health centers providing healthcare to medically underserved populations. What happens with the students who come in, many go into our clinics, and many times they change their whole focus and they want to become community health nurses or public health nurses, as opposed to going into pediatrics and others. Our community innovation program runs pilot projects that address health challenges in a new way and are addressing health priorities program and supplying local solutions to national health issues.
Dr. Lorina Marshall-Blake (00:24:22):
One of them is through, I call it our STOP program, Supporting Treatment and Overdose Prevention or STOP initiative, is focused on the opioid epidemic. We're responding to the COVID-19 pandemic by continuing to support community organizations that are providing essential health and human services. One of them that we're working with is called The Black Doctors COVID-19. It's a group of [inaudible 00:24:50] Dr. Ala Stanford, who now goes out into the community and does the testing in less than what, it hasn't even been two months, she's tested almost 5,000 people and she's going to areas and zip codes that traditionally, that folks don't go to. We've been very supportive of her efforts because we realize how important it is. It's not just one, it's all. In addition to grantmaking the foundation ran three campaigns in 2019. One was, Our Nurses Can, which was inspiring, empowering current and future nurses to pursue roles beyond the traditional care settings.
Dr. Lorina Marshall-Blake (00:25:31):
[inaudible 00:25:31] community highlighted the work of health centers in our region and the diverse community that is reached and served. I say, if you've seen one health center and we support 50, you've seen one health clinic, or one health center. They're all different, they're not the same. Then there is, Someone You Know, which was a grassroots public health awareness campaign, reducing the stigma of opioid addiction. Really, we went to change the narrative. We went to Washington, we took it to the halls of City Hall. We actually went back out into the community and we didn't tell the story. We had 20 ambassadors who told their story, what they were living with and what they were dealing with. Even in some cases, going back to what Barry was talking about, some of them were even homeless, but now are in a much more positive setting.
Dr. Lorina Marshall-Blake (00:26:24):
I'm working with a group called One Day At a Time. Again, it's about reducing the stigma of opioid addiction, inspiring hope, and empowering others to seek help and treatment. However, as I say, we are more than a check. We are more than just funds. I tell people, I don't just want to date you, I want to have a marriage. How can we work together and collaborate together and combine our efforts to make things better? Like our parent company, Independence Blue Cross, the foundation is the convener of diverse organizations, a force for new ideas. I'll tell my staff, "Nowadays people say, 'Let's think outside the box,'" to which I respond, "We don't have a box. Let's come up with something that really makes the difference, and it doesn't have to be what everybody else is doing." Again, we're a thought leader in addressing emerging health needs in the Southeastern Pennsylvania region.
Dr. Lorina Marshall-Blake (00:27:21):
It has been said, Margaret [inaudible 00:27:24] says, "Never doubt that a small group of thoughtful, committed citizens can change the world. Indeed, it's the only thing that ever has." I feel we have a responsibility to act as a leading voice to address the biggest challenges facing the health of our communities. We've leveraged the voice of our community, not only by speaking about the needs of the community, but by hearing, again going back to that, we need to listen. We should not be doing just the talking. We need to go into our communities and listen and hear what their concerns are and how we work together to affect change. But by hearing the needs of the community, funding through grantmaking, and actively participating in solutions to drive change and to shape public health in our region. I really believe we have a responsibility to do that.
Dr. Lorina Marshall-Blake (00:28:20):
We understand effective healthcare goes beyond what happens in your doctor's office. Again, going back to Barry, and if you're homeless, you don't necessarily have a doctor's office. One of the things about The Black Doctors COVID-19 is that they went directly to the shelters. They went directly to [inaudible 00:28:39] where the homeless were, and we were helpful in helping them get there with supplies and everything else that they needed. Our health is shaped by our community and the resources around us, or the lack of resources. The discrepancy in medically underserved communities are unacceptable. I'd like to highlight again, a few community organizations supported by the foundation who are addressing the health needs of individuals who are homeless.
Dr. Lorina Marshall-Blake (00:29:08):
While I focus on the support of the foundation, I want to begin by talking about a well-renowned nonprofit supported by Independence and the foundation. Many of you may already know Sister Mary Scullion, Project HOME, has helped thousands of people break the cycle of homelessness and poverty by providing a continuum of care. That's the key thing. You don't just stop and start, you're talking about a lifetime. This includes street outreach, supportive housing, and comprehensive services that focus on healthcare. They focus on education and employment through both adult and youth education and enrichment programs. Project HOME and its partners have pledged to end chronic street homelessness in Philadelphia. If you know Sister Mary Scullion, you know that's what she's going to do.
Dr. Lorina Marshall-Blake (00:29:57):
In January of this year, Independence, Project HOME, and AmeriHealth Caritas launched the Keystone Connection to Wellness, and initiative to address the significant health disparities in life expectancy and infant mortality experienced by North Philadelphia residents connecting Project HOME patients with resources beyond their immediate medical needs. With financial and operational support from Independence and AmeriHealth Caritas, Project HOME will work with other social service and health organizations to form a robust association of services to address social determinants of health. Additionally, this initiative will launch and facilitate a community advisory board. Again, you heard Barry talking about an advisory board, to help guide priorities and build on neighborhood strengths. Focused on improving health and quality of life for residents who live in two targeted zip codes of North Philadelphia. Again, listening and effecting change based on the conversation. This is one example of how we work together to address the impact of homelessness on health.
Dr. Lorina Marshall-Blake (00:31:07):
The foundation also provides grant funding through our Blue Safety Net program to Project HOME health services. With the foundation's support, Project HOME health services will expand access to high quality, low barrier health and wellness care to vulnerable and underserved communities. Another one that we work with is Pathways to Housing, is another amazing organization with a housing first model. Housing people directly from the streets without preconditions, then addressing any underlying issues around mental health, addiction, medical care, income, and education to help integrate and welcome them back into our community. The foundation support enhances Pathway's community-based treatment and support services for people with substance use disorder. For more than 15 years the Covenant House, Pennsylvania clinic, one of our Blue Safety Net grant recipients, has provided youth who are homeless comprehensive medical care in addition to offering housing and supportive services to homeless youth since 1972.
Dr. Lorina Marshall-Blake (00:32:17):
Lastly, I'd like to highlight one of our past grant recipients, the People's Emergency Center and 2019 Blue Safety Net grant recipient, Youth Services Inc. These two Philadelphia nonprofit agencies have a long history of providing critical services to children, families, and youth who are homeless in the city. Last year, they announced their strategic partnership. They decided to come together, take it in another word, vary again, to integrate services and provide a continuum of services that have a greater impact on those served. YSI's emergency shelter for homeless and runaway youth is one of only two shelters in Philadelphia serving boys and girls ages 12 to 17, and the only one to also offer medical services on site. As a Blue Safety Net grantee, the foundation's support enables YSI to continue to provide youth who are homeless with comprehensive treatment for all medical issues.
Dr. Lorina Marshall-Blake (00:33:20):
I had the honor and privilege of serving, some time ago, on the board of the People's Emergency Center that was founded back in 1972. They started then and they're still functioning. PEC is a comprehensive homeless services provider, an experienced nonprofit community development agency based in West Philly for parents, youth, and children who are experiencing homelessness. PEC provides the social services they need to improve their physical wellbeing, emotional security, and economic stability while they search for permanent or permanent supportive housing. The YSI and PEC affiliation creates a continuum of services for clients of both agencies. Making it will be much easier for clients to get the full range of support they need. Rather than have them go one place [inaudible 00:34:13] the other, it almost, to some degree it becomes one stop.
Dr. Lorina Marshall-Blake (00:34:17):
YSI and PEC currently work together in ways that against the city strategies to improve outcomes for children, youth, and families. While we are proud to support these community organizations through grantmaking, some of our best work happens outside of grant applications. We convene our grantees for annual partner meetings to facilitate discussions around important health topics. We are given an opportunity, again, to hear directly from them to listen. I think that listening piece is so important. We invite our grantees to contribute to foundation publications, such as the Journal of Change. We also have blog posts where we allow our grantees to write their story. We also focus our communications, not only on the work of the foundation, but on the work of the nonprofits we support, as ways we can drive through leadership, inspire, and educate together.
Dr. Lorina Marshall-Blake (00:35:15):
Collaboration is one of our guiding principles and our guiding principles are at the heart of all we do. All our work is made possible through a shared mission with our community partners. I think we will all agree that, as I said earlier, we can't do it ourselves. When I think about Chosen 300, which is another homeless group that we work directly with. It's partnering with them where they are and it's going to where they are. I don't wait for folks to come to 1901 Market Street, I go to where they are. I am often boots on the ground. We encourage you to learn more about how we actively participate in finding solutions to health issues by visiting our website. It's [inaudible 00:35:59] all the foundation's reports and publications, and by following us on Twitter and Instagram.
Dr. Lorina Marshall-Blake (00:36:05):
I will end with a quote from one of my favorite heroes, Dr. Maya Angelou, "If you find in your heart to care for somebody else, you will have succeeded." I often say, "Don't tell me you care, show me you care." I hope we continue to foster collaboration and connection to make a tangible difference in this world. Again, I thank you for the opportunity to present the Independence Blue Cross Foundation in work that we've been at since 2011. Thank you so much, and I'll entertain questions later too.
Cait Ellis (00:36:41):
Thank you so much for sharing Independence's leadership and longstanding history of supporting programs to help homeless individuals and for highlighting the critical role that partnerships and collaborations can play in addressing these major healthcare challenges and the value of listening directly to communities to really understand their needs. Our final speaker today is Christa Price, Program Director at True Colors United, an organization focused on the unique experiences of LGBTQ youth experiencing homelessness. Christa's commitment to advancing social justice is evidenced through her work, and we are so grateful she is with us today to share more about her organization's efforts to address youth homelessness during COVID-19. Christa.
Christa Price (00:37:27):
Thanks, Caitlin, and thanks to everyone, to my other co-panelists, Like Lorina said, I've learned so much from both of your presentations. My name is Christa [inaudible 00:37:40], and the work that we do at True Colors United, we try to implement innovative solutions to youth homelessness that focuses on the unique experiences of LGBTQ young people, like Caitlin said. Before we get started, I just want to take a moment to acknowledge the events of recent weeks and the systemic racism, homophobia, and transphobia that lead to the deaths of Tony McDade, Dominique Fells, Riah Milton, and [inaudible 00:38:11], four black trans folks who were recently murdered, because equity and housing justice is also anti-racist work. Systemic racism, homophobia, and transphobia also lead to homelessness, housing instability, and the disproportionate impact of COVID-19 on communities of color and LGBTQ communities.
Christa Price (00:38:36):
I also want to take a second, and I mean only a second because I don't have long, to highlight what we knew prior to COVID-19 about LGBTQ young people experiencing homelessness and youths of color who experience homelessness. We knew that LGBTQ and black communities are significantly overrepresented in the population of youth experiencing homelessness. LGBTQ young people are 120% more likely to experience homelessness than their non-LGBTQ peers. More specifically, black youth who identify as LGBTQ, especially young men, had the highest rates of homelessness. Youth and young adults are the second highest population to experience street homelessness after individual adults, meaning that they are less likely to have a safe place to stay or receive healthcare as my co-panelists have already mentioned.
Christa Price (00:39:39):
Then also we knew that there was a lack of sufficient rural housing services to allow for LGBTQ youth and young adults to be able to access emergency shelter in their communities or stable housing. Oftentimes, youth and young adults complained of not seeking housing services because they will be forced to move to a bigger city without any supports and/or anxiety of having to leave their communities to find adequate resources. We're seeing a significant decline of services in those rural communities. Then COVID-19 happened and we were in March. What we're seeing, we're seeing higher rates of COVID-19 infections in the black community specifically due to social determinants of health, like poverty, wealth, and access to healthcare. As the slide says, black folks are almost two and a half times more likely to contract COVID-19 than their white counterparts.
Christa Price (00:40:40):
We currently don't have any quantitative data on COVID-19 infections in the LGBTQ community. But anecdotally, we know that LGBTQ folks are less likely to have access to inclusive and affirming healthcare and will oftentimes forego healthcare for fear of actual or perceived discrimination. We're also, anecdotally, hearing about increased instances of domestic violence due to sexual orientation and gender identity. Again, we don't have any hard evidence on this and hard data collection on this in the past couple of months, but we feel like this is a direct result of young people having to shelter in place with unaccepting households, and also due to the fact that a lot of the social services designed to support them are closed. I know that there are a number of LGBTQ community centers that have closed across the country. Oftentimes those are, for LGBTQ young people, the first access to support services, including housing, that they have, that they seek.
Christa Price (00:41:53):
We also know that rural communities contain vast healthcare deserts including, in some places, where it takes over an hour to get to the nearest hospital, leaving LGBTQ folks no choice, but to try to navigate uninclusive healthcare system. This often results in a lack of cultural competencies among providers and nursing staff, doctors in rural areas for LGBTQ and black and brown populations, specifically around the disparities that impact these populations and how that contributes to the consistent practice of providers dismissing symptoms and/or not treating symptoms of these persons. As well as not addressing trans health optimally and instead treating trans patients based on biological compensation which contributes to inadequate care and just a lack of trust.
Christa Price (00:42:51):
We're also seeing a lot of economic implications for the community. We'll likely see the economic impacts of COVID-19 on the community for a long time. We know that LGBTQ folks and people of color are more likely to have lost employment during the pandemic. Homelessness is often a lagging indicator of recession, so we won't know for a while how this will impact rates of homelessness. But we are thinking that a year from now, we're going to see a significantly higher rate in homelessness. We're also anticipating even higher discrepancies for black men who have sex with men and trans women who are disproportionately affected by HIV. Anyone who is HIV positive and has lost health insurance will have a significantly harder time accessing lifesaving health support.
Christa Price (00:43:45):
Quickly, we're going to go through a couple of policy considerations. We encourage folks to continue supporting non-discrimination policies in provider settings. That includes the HUD Equal Access rule as it is. There were recently revisions made to the HUD Equal Access rule that allows shelters to set policies in which they make service delivery determinations based on their good faith assumption of biological sex, which is harmful to trans folks. Also in late 2019, HHS announced their intention to suspend enforcement of critical protections for discrimination on the basis of sexual orientation, gender identity, sex, and religion in HHS grants. Then the HHS 1557 rule that took effect Friday redefined sex as being non-inclusive of gender identity, which is also extremely harmful for the trans community. There are also a couple of state level policy implications, continue to support non-discrimination at the state and local level, especially in rural communities, given those implications.
Christa Price (00:45:03):
Then also, research and understand age-related barriers to healthcare. In a majority of the states, young people cannot consent to their own healthcare if they're under 18. At True Colors United we are looking at state by state broadly, age of consent rules or laws in healthcare. Then, support policies that holistically address the wealth gap, that will help with some of those economic implications that we talked about. Now is the time for that transformational change. What I think that means is that, if you're not centering the most impacted in your work or services, then you likely won't get there. A good place to start in centering the most impacted in your work, we have a couple of resources on that, is you can start with youth collaboration or client collaboration.
Christa Price (00:46:12):
For Pride Month this year, we're challenging all service providers to recommit to centering the most impacted in their work based on the data. If you're doing this work correctly, then it should include bringing black and brown LGBTQ folks to the table. We're featuring our free youth collaboration course for the month of June to help folks get started here. That is it. You can check out the Pride Challenge at the URL on the slide the bottom truecolorsunited.org/ 2020-pride-challenge. That's it for me. Thank you so much.
Cait Ellis (00:46:49):
Great, thank you so much, Christa for sharing your work and strategies to support the LGBTQ community, and for sharing what we do know about the impact of COVID-19 on this community. We would like to use the remaining time to engage in a Q&A session with our audience. Please continue to submit your questions in the Q&A tab. I'll also ask our other panelists to come off mute at this time so we can engage in a conversation together. To start, Bobby had mentioned Medicaid expansion, and for all of our speakers, we have had some questions come in around what other policy or systems changes could mitigate health and housing challenges of people experiencing homelessness.
Bobby Watts (00:47:37):
This is Bobby. I'll take a first stab at that, but one of the first things is that we need to recognize, not only healthcare, but also housing as a human right. We are, as a country, so far behind other industrialized countries in our policies in terms of recognizing those as rights and providing for the needs of our residents. Right now federal policy, or at least federal funding, is [inaudible 00:48:07] only for one out of every four households that qualifies for financial assistance to make their housing affordable in the form of Section 8 vouchers or other means only one out of four qualifies. Only one out of four that qualify receive that assistance. That's really just a matter of budgeting, and budgets are a matter of priorities, which is a matter of morality. That's one thing we can increase funding to make more housing affordable.
Dr. Lorina Marshall-Blake (00:48:44):
Okay, let me jump in there behind you, Bobby. One thing early on Caitlin had mentioned Dan Hilferty, who is their chief executive officer and president. Dan has been upfront with regard to healthcare being a right and the fact that, how Congress they need to move and move into that positioning. I think one of the other things that's important is to have, I call it a champion that can go out there, that has credibility not only in the industry, but across different industries and a consistent voice with regard to that. It won't happen overnight, but I think we just need to continue to express it, voice it. I think when you get folks that are... When you look at Independence, which is the largest healthcare provider in Southeastern PA, and where their president is saying that whether it's on Morning Joe, or whether it's on TV ads, or, again, upfront, I think that's the kind of leadership that we need with regards to that.
Cait Ellis (00:49:56):
Great. Thank you. Christa had mentioned the economic impact that we're seeing with COVID-19, the increases in unemployment, and we've had a few questions come in around, what should we be doing now to prepare for this, prepare for the potential increase in homelessness in the time period going forward?
Dr. Lorina Marshall-Blake (00:50:18):
I'll take that. I don't think there's a silver bullet to answer that question, but what I will say is that, as we look at the various nonprofits that are out there, that we're working with, one of the things we're working with is post-COVID, in other words, how we ensure that those nonprofits that have been working directly with [inaudible 00:50:38] whether it's Project HOME, whether it's Youth Services, whether it's the 50 health centers, that we ensure that they are there and sustainable in an effort to ensure that people have a place, A, to go for their health, but also for various services, even when it comes to workforce development and ensuring that there is a pipeline for it.
Dr. Lorina Marshall-Blake (00:51:02):
There's an organization called the Urban Affairs Coalition that we work with that has like 80 agencies that they work within the community, whether it's homelessness, workforce development, whether it's [inaudible 00:51:14], or whether it's opioids, whatever it might be. I think, again, that we need to ensure that they are there. Whether it's through funding or it's working directly with them or better yet, we get out there in the community and making a difference with regard to that.
Cait Ellis (00:51:37):
Yeah. Thanks. The only thing that I would add to that is, pointing back to what Bobby said earlier in terms of housing as a human right, as we see folks' income decreasing, nemployment increasing, et cetera, we really need to make sure that housing prices aren't continuing to increase. Supporting any and all efforts for affordable housing across the board.
Dr. Lorina Marshall-Blake (00:52:03):
Yeah. I think also making sure that there are rules in place or extension with regard to homeless, with regard to foreclosures. Again, working with the agencies that are out there that make sure that people don't end up homeless.
Cait Ellis (00:52:25):
Great. Thank you. We had a question come in and Lorina maybe you can start with that and we can open it up to the rest of the panelists. From your experience, what are some of the best practices in terms of communications and outreach strategies that we can use to reach homeless youth to help get them connected to health services and community resources?
Dr. Lorina Marshall-Blake (00:52:44):
Okay. Again, I'm going to say this, I'm one of those boots [inaudible 00:52:49]. When I look at what we do with regard to, let's take Covenant House, in that I have physically gone over to Covenant House, seen the young people that are coming in there, seen what their needs are, what their concerns are, how can we assist them. Connecting them with services and everything and all that they need. Again, I think, you can't, what is it? You could sit in the ivory tower, I'm not trying to sit in the ivory tower. We need to go out and actually be, when we say community, we have to be a part of the community and working directly with them. Not just when COVID comes up or when the pandemic comes. Not waiting for the crisis to happen, you need to become a viable part of that community that we live, work, play, and assist in. I've always been one that, no, don't tell me, I want to be there. I want to see what it is and how I really can have a real impact. I think mine is the best-
Cait Ellis (00:54:00): Would anyone else likeDr.
Lorina Marshall-Blake (00:54:01): [crosstalk 00:54:01] let me... The best practice is to be there, to be visible, to listen, [inaudible 00:54:08], in other words, again, not telling them, but actually listening and being open-minded and that acknowledging that you don't have all the answers. Guess what, unless you're there every day. It's one thing for me to say, "I did an event with Covenant House where I was homeless. I slept all night long on concrete." Again, that became even more real to me that, this is not... no one should have to be subject to that. I think, again, to the degree that people are in it, they're part of it. They're not just talking it, but they're walking it.
Christa Price (00:54:50):
Yeah. I would add to that, if young people are leading that work, then that will automatically fill those gaps. Like Lorina said, if you're working with young people, but if also, they are leading that work and informing that work, then those gaps will automatically be filled.
Cait Ellis (00:55:21):
Yeah. Great, thank you. We've spoken a lot about how COVID-19 and homelessness disproportionally impacts some communities. We've had a few questions come in around the veteran population. Is there any data on the impact of homelessness on the veteran population during the COVID-19 pandemic? Or rather, how has COVID-19 impacted veterans experiencing homelessness?
Bobby Watts (00:55:49):
That's a great question and I don't know the answer, but I will say that the country has made a lot of progress and efforts in addressing veteran homelessness so that as of now, I think at least 70 cities have said they have reached, a technical term, functional zero in veteran homelessness. Hopefully, because there are fewer homeless veterans than there were before, just by that they're not as affected. I just really want to point out what they provided to the veterans who are experiencing homelessness that worked was vouchers for affordable housing and services similar to the Pathways for Housing model which Dr. Marshall-Blake pointed out. That's, as far as I can surmise for veterans homelessness.
Dr. Lorina Marshall-Blake (00:56:47):
Again, I don't have any stats on it, but I know with the shelters that we've been involved with, a lot of folks are homeless. Amazing, often when I'm driving often there are veterans, their sign says, "I am a veteran and I'm homeless." Again, I mean, there's something wrong with the fact that you have served our country and done great things for us and you're homeless now. Again, I don't know what stats are, and we've done a lot of programs with veterans in an effort to get them, to bootstrap them back into the mainstream. There's a veterans home in Philly that we've worked with where we did, first off they were housed, and they housed like 34 veterans. That's the first thing, somewhere that you can go that you can call home, that you can have a sense of I guess, "I've got some place that I can live, that I can call my home." Again, then we gave them healthcare services and then started a computer program. Again, it's almost like rebooting them in an effort that they can go back and be self-sufficient.
Cait Ellis (00:58:08):
Great. Thank you so much. Well, we're coming up on the hour, so in our final minutes I would like to turn the floor back over to each of our panelists to share any closing remarks. If you would like to share anything about the most important lessons learned from before or during this pandemic and where you see us going from here. What are some of the solutions that are being implemented now that you would like to see continue or scaled up? Bobby, we can start with you.
Bobby Watts (00:58:35):
Sure. Thank you. I will just briefly say that some of the interventions that we have done during the pandemic, such as putting people out of shelters if they are a high risk, putting them into rooms, in hotels, or taking them out of encampments, putting them into rooms because they were seen a high risk, providing handwashing stations, toilets. These are things that we should have always been doing and that we should continue to do in order to prevent the next epidemic.
Dr. Lorina Marshall-Blake (00:59:06):
Yeah, I agree. I agree. I would say that it's important as funders, whoever we are, our foundations, that we get out there and we see exactly what's going on. I come back to, I love quotes, and one of my favorite quotes is another one by Dr. Maya Angelou where she says, "People won't remember what you said, and they won't remember what you did, but they will always remember how you made them feel." Even though you're homeless, that does not mean that you don't have a voice and that you don't matter. I think it's important that people know they may... I think someone talked... Bobby, I think you talked about it earlier where homelessness is temporary. Stop looking at it as just for the moment. In other words, we can move to another level. It's not a permanent state. I think to the degree that we foster that with our program, and with our dollars, and working with the community. That would help.
Christa Price (01:00:11):
Yeah. I look at it from True Colors United perspective, something that is near and dear to our work is that [inaudible 01:00:18] collaboration aspect. As much as folks can, make sure that you're centering your clients, the people that you work for, the people that you serve, in the work. They should be informing programs, they should be informing policies, they should be informing the work as a whole on all different levels. That's hard work to start, to do, and we could help. Yeah.
Cait Ellis (01:00:48):
Great. Thank you. Well, with that, I would like to thank our excellent panel of speakers for being with us today and sharing their great work and thank you to our audience for engaging with us today. Feedback is important, so please take a moment to complete a brief survey which can be found on the bottom of your screen. Thank you all again for joining us.
Presentations
Health and Homelessness - Before and After COVID-19

Bobby Watts, MPH, MS, CPH
National Health Care for the Homeless Council
Collaboration and Connection

Rev. Dr. Lorina Marshall-Blake, MGA, FAAN
Independence Blue Cross Foundation
NHCHC COVID and Medical Respite Resources
- Material on COVID
- Medical Respite Care Program Directory
- Respite Care Providers Network
- Policy brief: Medical Respite Care: Financing Approaches
- Policy brief: Medical Respite Care Programs & the IHI Triple Aim Framework
- Policy brief: Managed Care and Homeless Populations: Linking the HCH Community and HCH Partners
- Technical Assistance requests
More Related Content
See More on: Coronavirus | Social Determinants of Health