Webinar
COVID-19 and Mental Health in the Workplace: Solutions for Employers and Employees
Time & Location
The COVID-19 pandemic and resulting economic recession have negatively affected the mental health of many Americans. The number of adults reporting that stress of the pandemic impacted their mental health increased from one third in March to over half of adults in July. The mental health consequences of the pandemic are widespread and impact everyone from frontline and essential workers, to those working from home.The pandemic has also highlighted unequal access to behavioral health care. While their rates of behavioral health disorders are similar to the general population, Black and Latino people experience greater barriers in accessing mental health treatment.
This webinar brought together experts to discuss the opportunities and challenges that the pandemic poses for mental health and workplace well-being. Speakers discussed:
- The trend of declining mental health in America before and during the COVID-19 pandemic and what needs to be done to ward off a mental health crisis in the future
- What a large employer and health plan is doing to prioritize mental health among its employees and members
- How a community-focused organization is improving mental health and mental health awareness in the Black community
Cait Ellis (00:00:00):
Good afternoon. I'm Cait Ellis, program manager at the National Institute for Health Care Management Foundation. On behalf of NIHCM, thank you for joining us today to explore this important topic.
Cait Ellis (00:00:11):
This is a challenging time, and our goal today is to share information and actionable strategies to support mental health in the workplace. As the COVID-19 pandemic continues, Americans are facing mounting mental health challenges and stressors. While the pandemic has impacted everyone differently, over the last eight months we have seen workers face unemployment concerns, challenges with childcare or virtual learning, fears of getting sick, and struggles maintaining a work/life balance. All of these factors can weigh heavily on employees and significantly impact their mental wellbeing. Recent surveys have shown that symptoms of anxiety and depression have tripled and quadrupled during the pandemic respectively.
Cait Ellis (00:00:55):
This expert panel will discuss short and long-term strategies to address mental health challenges and explore opportunities for employers to insure that these mental health challenges do not turn into serious, long lasting mental health problems. Before we hear from them, I want to thank NIHCM's President and CEO Nancy Chockley and the NIHCM team who helped to convene this event. You can find biographical information for all of our speakers on our website, along with today's agenda and copies of slides. We also invite you to live Tweet during the webinar, using the hashtag #workplacewellbeing.
Cait Ellis (00:01:33):
I am now pleased to introduce our first speaker, Dr. Kathleen Pike. Dr. Pike is a professor of psychology at Columbia University and serves as the director of the Columbia WHO Center for Global Mental Health. She brings extensive experience and expertise to this topic, including her work designing and delivering mental health services in fragile and post-disaster settings, and a recently announced partnership with Maybelline New York to confront mental health issues and stigma. We are so grateful she is with us today to share her work and perspective.
Cait Ellis (00:02:04):
Kathy?
Kathleen Pike (00:02:05):
Thanks so much. It's really a pleasure to be here and I appreciate the opportunity to join the discussion.
Kathleen Pike (00:02:18):
So, why does mental health matter in the workplace? Mental health has always mattered in the workplace. We know that mental health is significantly associated with productivity and work performance, we know that good mental health is associated with reduced absenteeism, turnover, and injuries. We also know increasingly that the extent to which companies pay attention to mental health and wellbeing of their employees is associated with enhanced reputation, recruitment, and retention. And it is very clear that mental health is very much centrally associated with other health conditions that are relevant to employees, including things like diabetes and heart conditions.
Kathleen Pike (00:03:12):
So, that's always been true. What's happened now is... I'm just waiting for the next slide... is that with COVID-19 we've got a range of significant new stressors or exacerbated conditions that, in our research, has emerged as the most significant variables associated with the rising mental symptoms. The ten COVID-19 stressors that are most relevant, from our work looking at mental health and work during COVID-19, have to do with the very high levels of ambiguity and uncertainty associated with the pandemic, the overwhelming amount of COVID-19 related information in the media, and the conflicting information. The third point, the real risk of infection is a very significant stressor. The fourth stressor, related to physical distancing and the associated social isolation, have very serious mental health repercussions.
Kathleen Pike (00:04:30):
The fifth variable is the change in work demand, work structure and processes. This has varied significantly, depending on the type of employment that someone has, but each of those has significant risk in terms of mental health. Increasing the changes in domestic responsibilities that increase stress or impede work, and in particular the issues around work from home and the impact for employees who have children who may or may not be in school, or have older parents who may or may not be living with them, or in senior residences has put significant stress on employees.
Kathleen Pike (00:05:26):
Of course, having a loved one with COVID-19 or losing a loved one. And studies are showing now that given the rates of individuals in the U.S. who have died from COVID-19, that we literally have over two million Americans who are grieving right now, having lost a parent, a child, or a partner. The financial concerns and job security are associated with significant concerns and worries that increase mental health risk. The worsening of comorbid long-term health conditions that are being impacted by reduced access to care or concerned about seeking care. And then, tenth, there are significant increases... employees are reporting significant increases in terms of privacy and confidentiality with employers now tracking where they have been, where they... who they are in close contact with, et cetera.
Kathleen Pike (00:06:39):
When we look at the... what those stressors translate into in terms of stress, a few significant numbers. An estimated annual cost of mental ill health to our U.S. economy is $260 billion. 96 percent of all U.S. adults say the pandemic has impacted their overall stress. 80 percent of respondents... when we look globally, 80 percent of respondents in India felt the need for increased mental health services and access. 42 percent of respondents in the UK report significant increases in terms of fatigue due to the lockdown. And the bright side of this story is that we know that if we invest in employee mental health, for every dollar invested, we have a return of $4. So, it's a really good investment, especially at a time of these increased risks.
Kathleen Pike (00:07:48):
Within the U.S., the most recent data from the CDC indicate that about 40 percent of Americans, American adults, report struggling with mental health issues. That common mental health issues are around anxiety, depression, trauma related risks, increased use of substances, and even some increase in terms of suicide. These increases in symptoms have led to major headlines that I'm sure many people have seen in the media around warning about the next pandemic and the shadow pandemic of mental health. And what I want to say, loud and clear here, is that the elevated rates of mental health concerns are very serious, but a mental health pandemic is not inevitable.
Kathleen Pike (00:08:52):
What we can learn from the data from... what we want to consider here is that elevated symptoms are not mental health disorders. And, in fact, when we think about people reporting that there are increased rates of anxiety, or fatigue, or concerns about employment, or trouble sleeping, those are pretty normal responses to a very serious global pandemic. These are feelings that alert us to the seriousness of the problem, and even motivate us to do what we need to do in response to a very real problem, like wearing masks, and avoiding large gatherings, and so on. Normal, appropriate emotional responses that we can consider signals, in the same way that feeling when we go outside and it's cold, we put on a coat in the winter. It tells us that we need to bundle up, right?
Kathleen Pike (00:10:02):
The key consideration here is not that people are feeling increased symptoms. The question is, what is the severity of the symptoms, what's the duration, and what's the impairment? And when symptoms become extreme in terms of severity, when they endure over significant periods of time, and when they interfere with daily functioning, that's when we know it's time to intervene.
Kathleen Pike (00:10:33):
So, what do we know from other public health crises? This slide shows us some data from two different moments in history that offer some guidance. The first row, here, looks at the mental health sequela after 9/11. What was the prevalence of post-traumatic stress and related mental health conditions after the September 11 attack in Manhattan? One month after September 11th, the rates of mental health concerns were significantly elevated, to 7.5 percent of New Yorkers reporting increased levels of mental health problems. But six months after 9/11, rates had gone way, way down.
Kathleen Pike (00:11:26):
Another point of reference for us is to look at the second row of data, which represents information around mental health from epidemics and widespread public health crises from the 21st century, including pandemics and epidemics of SARS, Middle East Respiratory Syndrome, Ebola, and Swine Flu. And what we see here from these data, from a review of these data, is that immediately after an epidemic or pandemic, we see significant range in terms of mental health response. And unlike 9/11, even a year later there are significant elevations, but also very significant range.
Kathleen Pike (00:12:17):
So, the take away here is that when we have these health conditions, these major public health conditions, we're going to see a very wide range of response, and we're going to see that the response has more of a lasting impact.
Kathleen Pike (00:12:35):
Who is at most risk and what accounts for some of that variability? What we want to keep in mind is that the individuals who are going to be at most risk for the elevated mental health issues are those who have preexisting conditions, the intensity and severity of exposure, and the amount of support that they have from within their community and contacts. Those factors are going to mediate the mental health response.
Kathleen Pike (00:13:10):
So, what can leaders do during this time? Our data show that leaders play a very, very significant role, have an outsized opportunity in terms of shaping the organizational response and impacting the mental health outcomes. Eight key steps for leaders. Communicating clearly and often, making mental health a normal part of the conversation, recognizing that it is part of this pandemic. Leaders have an opportunity to facilitate peer and team support. Leaders have an opportunity to promote and model flexibility that will be essential given the stressors of this enduring pandemic. Leaders need to support open, two-way conversation, not only reporting out, communicating out, but creating channels to hear back from employees, especially given the way in which teams and work forces have been fragmented. Leaders have the opportunity to normalize employees' heightened anxiety. Leaders have the opportunity to remind employees about the importance of mental health, and they have an opportunity to promote and model self-care.
Kathleen Pike (00:14:30):
When we talk about organizational strategies, we often, in our consulting work with organizations, we talk about the three Ps. Leaders have an opportunity and an obligation to protect employee mental health, to promote positive mental health, and to provide access to appropriate care.
Kathleen Pike (00:14:52):
What do we mean by protecting mental health? What leaders have the opportunity to do there is prevent exposure to undue stress and situations that could cause mental health symptoms and problems. Right now that includes things like creating flexible work hours, addressing family leave needs, cultivating a culture of trust. Those are protective strategies to reduce mental health symptoms. Leaders can also promote good mental health that enhances skills, resilience, and coping. What does that look like today? It looks like creating routines and structures amidst uncertainty, it means building peer support groups, it means skills building workshops, it means modeling self-care. That's a strength based approach that makes an enormous difference at times of enduring stress when individuals are at risk for mental health symptoms.
Kathleen Pike (00:15:54):
And then, third, leaders need to provide opportunities for employees to talk about mental health needs and to access care as needed. What does that translate to today? Knowing what's available within your organization, facilitating connections to resources for employees who are struggling with mental health concerns, and expanding resources as needed.
Kathleen Pike (00:16:20):
What's critical at this moment, which is critical always, but especially at times where there are increased stresses, increased uncertainty, increased ambiguity, increased needs and increased efforts, it is all the more important that leaders are very, very clear about the problem that your trying to solve for right now. What are the mental health issues in your organization? Define the problem clearly. You need to articulate success. What will success look like if you address the mental health problems. Make sure you measure and learn, innovate and iterate, and then go back to defining the problem. The biggest mistake that we see at times like this is that programs get developed without clarity about what the real problem is and what success really looks like. And the result is significant efforts without clarity of outcomes, and then we don't know that there's really been desired impact. And we just can't afford that at the moment.
Kathleen Pike (00:17:32):
So, the take aways for today, in terms of our big picture, is that mental health consequences of COVID-19 are vast and serious. A shadow pandemic is absolutely not inevitable, fortune favors those who prepare. And there are ways that organizations and organizations with strong, clear leadership can address the mental health needs so that employee mental health is protected, that the employees' mental health, positive mental health is promoted, and that for those individuals who have more serious mental health needs, appropriate care is provided. Employers have an enormous opportunity to support employee mental health during and beyond COVID-19.
Kathleen Pike (00:18:25):
And I look forward to hearing from my fellow panelists about the work that they are doing to address mental health in their organizations. Thank you very much.
Cait Ellis (00:18:38):
Great. Thank you, Dr. Pike, for giving us some background on common stressors that we're seeing, providing such thoughtful context around how the pandemic is impacting mental health for workers in the United States, and exploring what can be done to help avoid a mental health pandemic.
Cait Ellis (00:18:56):
Under the leadership of Gail Boudreaux, Anthem is investing in addressed mental health challenges and providing relief and resources where they're needed most. We are pleased to have Brad Lerner, Anthem's Health Policy Director for Behavioral Health, with us today to share more about their efforts. At Anthem, Brad analyzes state behavioral health legislation and regulations, and works closely with the Federal government relations team to support strategy and advocacy. We appreciate him joining this panel discussion to share [inaudible 00:19:29] and his perspective.
Cait Ellis (00:19:31):
Brad?
Brad Lerner (00:19:34):
Hi. Thanks everybody, and thank you, Dr. Pike, for some very thoughtful statistics and information that I think will build nicely on my slides. I appreciate NIHCM for giving me the opportunity to speak here today.
Brad Lerner (00:19:48):
Just a little bit about Anthem before I get in here to the slides. As was mentioned, this is a large health payer that focuses on employer business and employee wellbeing. Recently, prior to the pandemic, Anthem acquired Beacon Health Options, which is a wellness company singularly focused on behavior health. So, it was fortuitous that Beacon is now part of the Anthem family and we can work on solutions together, helping employers during this really unique and trying time.
Brad Lerner (00:20:24):
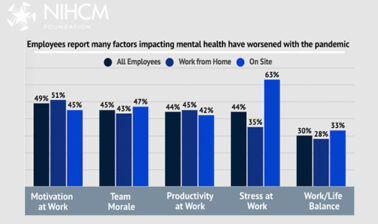
So, I did put some statistics in here, as well, but I'm not going to spend a lot of time because I think Dr. Pike did a really nice job of sort of setting the moment in time that we're in, the tremendous pressure that employers, and individuals, and employees are feeling. So, these slides will be made available to you, but as you can see, mirroring some of Dr. Pike's comments, we're seeing just increased rates of depression, self-reporting on just overall stress. We are focused on stress of working at home, particularly folks who are living alone. There's the social isolation, just getting used to this whole transition of how we work is causing tremendous stress.
Brad Lerner (00:21:17):
We're also, as an employer, always looking for employee... as employers looking at productivity, and what is this... trying to measure what is the impact of the mental health needs of employees during the pandemic. And you can see that there's increased stressors, and that the U.S. is particularly increasingly focused on... in surveys on having the highest sort of mental health distress results when surveys are taken.
Brad Lerner (00:21:46):
So, I think a good place to begin here, too, is pick up on Dr. Pike's, what do we want the workplace to accomplish? We have all this uncertainty, anxiety, isolation, I think people are looking for that resilience, we've done resilience training in the past. Never before will we need to call on it and how are we going to bolster that? And I think employers have to rethink strategies that particularly on each of the strong stressors we're seeing. So, I really like this slide here, in that it's focusing on some results on how to reset work expectations and just sort of adjust the relationship. Maybe there's more communication that's going to be needed, and more ways of unique social engagement.
Brad Lerner (00:22:35):
So, that sort of sets the tone, I think, between the two speakers here. You see that we are in a trying time, but what has Anthem and Beacon, what have we done as a result, what happens in order to help the folks with mental health needs, the employers and employees? So, telehealth is really the large story for mental health here. It is the leading diagnosis that are for telehealth visits are stressing anxiety and depressive disorder. The telehealth use is 110 times higher.
Brad Lerner (00:23:10):
We're also seeing that we're reaching people who are managing to be inpatients. They're staying for longer, they're coming in at a higher acuity than previously before. We have seen some evidence of increasing suicidality, and increasing needs on social determinants of health. That's a term, if folks aren't familiar with, where we're really looking at how the interplay of people needs for food, transportation, living arrangements, impacts their mental health.
Brad Lerner (00:23:40):
I'm going to keep going here. So, what did we do? There's a lot of information here, but what was actually done? Well, that telehealth story really was something that... telehealth existed prior to the pandemic, telehealth for behavioral health was always something that was thought of as a good fit for telehealth. It's not like you could set a broken bone, this is something where you don't have to touch the patient. There should have been... there has been evidence that it works in the outpatient for the non-severely mentally ill.
Brad Lerner (00:24:17):
So, when you had that rapid shift where, in the early days of the pandemic, where people were really told not to leave their homes, we saw an incredible sort of industry... a lifetime of industry work happening in a quick time. And one of the things that Beacon and Anthem did was focus on training for our providers. It wasn't intuitive for everyone to just be able to move to video, face to face chatting. And we decided to... we had held a number of trainings early on, whether it was technology or billing or what is proper practice, and we really helped to lay that groundwork early on, and it's continuing to grow the sort of treatment of mental health and substance use conditions.
Brad Lerner (00:25:06):
Even early on there were new modalities for treatments that never before had been treated over telehealth. So, you had some of the more intensive treatment levels, like intensive outpatient treatments or partial hospitalization, those were exclusively... applied behavioral analysis for autism, children with autism, all of these were done early on in the pandemic over virtual sort of mediums. Now we've seen some moving back to the traditional face to face, but being able to have that ability to have that continuity of care was really important for our members. And I think it was very important for employers, to make sure that they felt that their members were getting the treatment in real time.
Brad Lerner (00:25:54):
One of the things that we're also seeing is that there were... in order to make this sort of telehealth work, we saw a lot of flexibilities that were added, that sort of bolstered the ability of providers to use telehealth. So, some of the rules that existed before about how... where you could do telehealth, whether you had to do it from your home or at a different location, whether you had to have an established patient, there was definite licensure flexibility for providers to sometimes do treatment across state lines. So, different things were lifted that we're going to want to look carefully at as the pandemic continues and beyond, to see about these flexibilities continuing because it really helped proliferate the use of telehealth.
Brad Lerner (00:26:44):
And we also, just as a... we really had to rethink some of our care. A lot of... when you do sort of virtual care and we were moving away from face to face early on, that we had a lot more care management, a lot more proactive outreaches. We had to have more in the moment support. We also looked at different ways of communicating information. So, there was a lot of sort of industry wide changes that occurred in a short period of time to really bolster the mental health needs of our consumers and our members.
Brad Lerner (00:27:16):
Take a little pause here. So, we just, again, tried to get the word out, a lot of information put on different websites, social media, podcasts, articles, you name it, I think just key with employers and employees was making sure that we can meet the people where they were with the information they need. Obviously, the web was an incredible source of information for folks who were struggling.
Brad Lerner (00:27:45):
And I thought I'd get into a few of the programs that Anthem and Beacon sort of mobilized. So, when we have our employer business, there was a lot of concern about employees' mental health states and what could we offer them immediately, whether they were, sort of as Dr. Pike had mentioned, not even the severely mentally ill, people who were just under tremendous stress, what could we offer them? And there was always for our employers employee assistance programs, and we wanted to make sure to direct employees who had those available to them. Those offered quick sessions, you could do five sessions via the phone or via telehealth, and be able to sort of get your anxiety, and discuss the issues maybe of childcare or all the things that were sort of the immediate stressors.
Brad Lerner (00:28:39):
We also implemented some additional programs and a few of them are listed here. PsychHub was interesting. PsychHub was something that we partnered, that was a free digital resource for our members, to help them help providers learn about mental health and give them some mental health treatment options right off the bat. Some more personalized applications were given to members, such as myStrength, which helped connect people to sort of give wellness and tips. And we had auntbertha, which is on here as well. That was helping with sort of social services, connecting folks. Sydney Care was something that was implemented to help members when they had symptoms and get them quickly into primary care, which was really important during the early days of coronavirus. So, a suite of products and options. LiveHealth Online was the treatment with full-on therapy treatment that you could do virtually, that would be across the whole footprint.
Brad Lerner (00:29:46):
So, these sort of tools and resources, immediately trying to respond to the pandemic and all of the statistics to say, hey, if you're an employer, how do I keep my employee healthy? We wanted to make sure that people had the right tools available to them.
Brad Lerner (00:30:07):
What to expect. I think that we really wanted to make sure that we're following what's happening. I think nobody really knew how long the pandemic was going to last, how long folks were going to be at home. And now we're sort of seeing in the news another uptick in cases. And with that, I think again, people constrict their care. And we want to make sure, with the projections, that people are feeling increasingly stressed, but if they're afraid to go get treatment or don't know that they have these virtual options available, we want to make sure that they don't show up at the hospital at an already highly acute rate. So, we want to make sure that we reach them early, and we're trying to think of ways to make sure that we're checking in with our members, our employees through our employers, to make sure that they are well-prepared for the winter and know that they have those options that I mentioned available, where you could do sort of real time treatment from your home or at least get... and the ability to talk to somebody early on, through your employer. Just even go through how you're feeling.
Brad Lerner (00:31:16):
So, we want to avoid that sort of high level acuity where it got too far. I think one of the... Mental Health America talks about Before Stage IV. And I think even in a truncated pandemic, we definitely have a Before Stage IV situation going on here. We're all sort of struggling. So, we want to make sure that we give folks the tools to reach people before it becomes more acute. So, some of those projections are in there.
Brad Lerner (00:31:45):
We expect that telehealth will continue. It is a really key piece of the... I don't want to say it's a silver lining, but something that's been building up for a long time for outpatient treatment for anxiety, for depression, using that sort of two-way medium. And it always made sense for a lot of businesses to take advantage of it. I know that we used to have folks who were on oil rigs, that were distant and couldn't necessarily get to treatment. And it made sense, but it was just not really well taken up. And now, all of a sudden, we see this was the sort of nail that hit it over. And I believe that with these... the key thing that we're going to be working towards is making sure that the policy makers continue to relax regulations to make it easier for the mental health patient, particularly in mental health telehealth, to continue to use telehealth through the pandemic and even beyond.
Brad Lerner (00:32:42):
So, we really expect demand to continue, so that sort of relationship between having the telehealth capabilities and keeping our eye on the mental health needs of our members and consumers and employers.
Brad Lerner (00:33:00):
And then, I'm going to go finish up here. Again, employers really increasing the benefit, making people more aware than ever. A lot of people weren't even aware they have employee assistance programs. Now is certainly a time to take advantage of that. Making employees aware of the telehealth benefits, that they may not. Even making them aware that they have mental health benefits. So, these are things that are tangible steps employers can take.
Brad Lerner (00:33:27):
And then, in the last slide here before I hand it over to Yolo, is just, again, the adjustment. We really want to emphasize the telehealth, emphasize the EAP, make sure their webs have abilities to highlight these programs. We, at Anthem, want to make sure that we're doing virtual peer support, have resiliency tools, cognitive behavioral therapy tools. Employers can, again, incentivize different ways going forward to cover behavioral health that may increase uptake either through different cost sharing arrangements. Other employers may look to work with clinics, either on-site or nearby. And making sure that front line managers, business agents, benefits, that there is this sort of training. There's mental health first aid training that we really support at Anthem.
Brad Lerner (00:34:29):
So, I think there's a lot of options out there for employers, that we can work with you and make sure that we are on top of this as it continues to develop. And it does not look like we're going to have a near-term fix, so we really want to make sure that we make sure that all of these tools are available to our population.
Brad Lerner (00:34:50):
So, with that, I'm going to look forward to some questions from folks. And I will hand it over... back to the moderator for Yolo's remarks.
Cait Ellis (00:35:01):
Great. Thank you so much, Brad, for highlighting the emotional toll that COVID-19 is having on employees, outlining some specific tools and resources Anthem has made available during the pandemic, and giving some concrete examples of what employers are currently doing and what they can do going forward to better support their workers.
Cait Ellis (00:35:20):
Our final presentation will be from Yolo Akili Robinson, Founder and Executive Director of BEAM, The Black Emotional and Mental Health Collective, an organization dedicated to removing the barriers that Black people experience around mental health access and support. Yolo was recently awarded the prestigious Robert Wood Johnson Foundation Health Equity Award for his work. We are so fortunate that he can be with us today to share in this conversation.
Cait Ellis (00:35:45):
Yolo?
Yolo Akili Robinson (00:35:48):
Yes, thank you so much. So, first let me just say thank you to my co-presenters for really offering a little background and framework for me to have this conversation. And also, of course, to NIHCM for inviting me to be a part of this dialogue. It means a lot to have our work as a part of this discussion.
Yolo Akili Robinson (00:36:06):
As you shared, my name is Yolo Akili Robinson. I'm the Executive Director and founder of BEAM, The Black Emotional and Mental Health Collective. BEAM is a national training, movement building, and grant making institution, as was shared. And what I'd like to do today is actually talk a little bit about our work, and our approach, and our motto as it comes to addressing mental health, as well as kind of highlight some specific things that I think can be helpful in terms of thinking about mental health in the workplace from a healing justice theoretical approach and perspective. And I'll talk a little bit about what that is in a moment, as well.
Yolo Akili Robinson (00:36:41):
So, [inaudible 00:36:42] using the tool right. Okay. So, I want to talk about first the three buckets of our work, which will really be a great way to kind of understand how we conceptualize and understand mental health first of all. So, the first piece of our work is... BEAM is primarily a training institution, but our training is built on the premise that we can't just rely on psychiatrists, social workers, or therapists for our communities to heal and be well. In fact, when it comes to Black communities, we recognize that very few of us actually do rely on those institutions as they're often interconnected with the criminal legal system that seems to continually create a lot of violence and harm towards Black and brown communities.
Yolo Akili Robinson (00:37:19):
And so, understanding that, we recognized that we need to do something called village care. We recognized that the people who are on the front lines of emotional health and support in our communities are often not those social workers and therapists, but are often teachers, coaches, educators. They are often activists, big mammas, cousins, family members. And that when those folks have the support, skills, and tools to be able to support... to show up, then our communities are able to cultivate wellness. However, when those folks are barriers to care, they can become... they can increase systemic barriers and really keep people from getting access to their needs or their wellness, right?
Yolo Akili Robinson (00:37:55):
One story that I often tell that kind of emphasizes why we do the work and the approach of the work that we do is, there's a story about a young woman who was living in the rural South. Got a diagnosis from a clinician of living with bipolar. However, once she got that diagnosis, her family and her religious community rejected that diagnosis and told her that that was not genuine, that was not real. And so, because of that she suffered many of the different challenges of what it's like to live with bipolar untreated for several years. Until one day she was sitting down with a stylist who was doing her hair, and the woman tells her... and she shares with her about her diagnosis at one point and also her family's response.
Yolo Akili Robinson (00:38:32):
And the stylist says, "Well, hold on, that doesn't make any sense. I have a cousin who has lived with bipolar, let me tell you what she went through. And you can't listen to those people because that's not true." And gave her a different narrative, a different story, and due to that she was able to actually get access to treatment. She was encouraged to get access to treatment, got access, and actually was able to show up in her own body and in her own life in a more, in her own words, in a way that was more indicative for herself.
Yolo Akili Robinson (00:38:57):
So, this is one of the reasons that our training and our education really focuses on village care, and training folks who are not just clinicians, but people in every aspect of the community, to really be able to do what we call healing justice peer support and show up for our community.
Yolo Akili Robinson (00:39:12):
A part of when I say healing justice, I want to make sure... that term may be new to people. Healing justice is a theoretical approach to healing and wellness that is rooted in the activism of Black, queer, trans, disabled, women, and gender nonconforming folks from the South. It really situates that we could not heal until we actually address the core issues in our society that perpetuate unwellness, whether it is a commitment to hyper-productivity, whether it's capitalism and how sometimes capitalism can create harm and pain, whether it is also racism, sexism, homophobia, and all these other systems that are interconnected. So, it is not about treating the symptoms, but also addressing the core issues that create so much distress in Black and brown communities.
Yolo Akili Robinson (00:39:53):
And so, our training approach is really centered on that particular piece, right? So, when our barbers, when our educators, and our counselors have those skills and tools, then our community is able to cultivate wellness in conjunction with mental health professionals as well.
Yolo Akili Robinson (00:40:06):
The next piece I'll talk about is our grant making and our community organizing, very briefly. We believe in building upon and expanding ideas for what constitutes mental health. The medical model often says the only mental health work that's being done in this country is being done by people who are clinicians, who are psychiatrists. We reject that. We recognize that when Black Lives Matter activists are out in the streets advocating for an end to police brutality and the murder of Black and brown people, that that is a mental health intervention. It is addressing our anxiety, our depression, it is addressing the stress that's fueling a variety of different mental health symptoms in our communities, right? And so, we recognize and expand our understanding of wellness and mental health to be beyond the medical model, while also emphasizing the brilliance and expertise of mental health professionals, but also challenging the systems as well for some of the ways in which they can perpetuate racism, sexism, and inaccessibility.
Yolo Akili Robinson (00:40:56):
So, we fund everything from doulas doing birth work support for Black women, we fund herbalists who are doing herbal medicine for our communities, we fund people doing barbershop education because we feel like, once again, it has to be on different pieces and elements.
Yolo Akili Robinson (00:41:10):
Third piece I'm going to talk about, which is... really kind of helps build upon what I'm here to talk about, organizational wellness. So, we talk about organizational wellness in this particular moment, we, as you might have garnered already, take a little bit of a more of a radical approach in terms of thinking about what... how do we actually cultivate wellness for our institutions, and our systems, and our community based organizations? How do we help them center healing? How do we actually help them actually effectively address racism, sexism, and integrate restorative or transformative justice practices into their work?
Yolo Akili Robinson (00:41:44):
Understand that this is not going to be an eat, pray, love moment. It will not be sensitive, and lovely, and always beautiful, it will be difficult because it will be long-term. It will require a deeper kind of engagement with the work. And so, a lot of our work has going in-house with the institutions. Some corporate institutions are primarily community based and grass roots institutions to really help them to cultivate wellness for the folks who work there, but also for how they deliver services for the folks who work there as well.
Yolo Akili Robinson (00:42:12):
So, that being said, I'm just going to briefly... I think I'm going to skip to Slide 6 actually. So, let me just talk about some things that we've been encouraging folks to think about when it comes to cultivating wellness in the workplace. And I can imagine people seeing this slide being, "Okay, he's going to go there." Yes, I am.
Yolo Akili Robinson (00:42:31):
So, the first thing I think that's really important when we're talking about racial justice, or we're talking about economic justice, we need to talk about the fact that during COVID, in this particular moment, the reality is that many people have lost their jobs. And there are many institutions that have staff who are supporting multiple family members who have lost their jobs. For example, there are many of our clients report that high percentages of their own staff are supporting, paying rent for their parents, paying rent for cousins, paying rent for grandparents who have lost income that they had prior to this particular moment because they were in the service industry or doing a variety of other kind of economic ways they were getting money that's no longer available to them.
Yolo Akili Robinson (00:43:16):
So, we talked to organizations about giving bonuses to staff as a way to help support wellness, right? To actually help support their long-term investment in their staff, but also helping support people's mental health because economic stress is a real issue right now.
Yolo Akili Robinson (00:43:32):
The second one I want to talk about is reassessing workloads and expectations on productivity. We, in this country, have ridiculously high and unhealthy ideas of productivity that have to be interrogated at the core, right? They are deeply rooted, sometimes they're very ableist concepts and very racist concepts. And often, not really equivocated or connected to how people are being compensated very well, right? And so, one of the things I tell people when I work with executive directors is, "The first thing we have to understand when you're in a leadership role, whether you're a manager or an executive director, is that you hold such... the way you model, the way you lead either helps or hinders the mental health of the people who are in your institution."
Yolo Akili Robinson (00:44:14):
And so, it's really critical that when we're in this moment we understand that we are working through a crisis, and that our crisis is going to have a diminished... it's going to diminish the impact in the ways in which we're going to be able to show up. So, we need to reassess workloads and expectations of productivity. We need to be realistic. We need to really realign and reimagine. Some of the simple things I put here, like stopping compulsive Zoom meetings. I can't tell you how often I'm going in house at institutions or organizations and everything is now a Zoom, it's become almost compulsive. And actually, instead using Zoom time for integrated, intentional, really building relationships, not just because I need to jump on a call for this one small thing, right?
Yolo Akili Robinson (00:44:56):
It actually is exhausting. We're experiencing a lot of fatigue because we are now sharing space with people in ways we were not sharing space. You're seeing people's homes, people's bedrooms, which produces a little bit of anxiety, right, and frustration for people. So, really acknowledging that and stopping that particular piece.
Yolo Akili Robinson (00:45:12):
Challenging compulsive urgency anxiety. I think the nonprofit industrial complex really struggles some with urgency anxiety or urgency addiction is what people call it. Really being able to... we have a couple of tools we share to really help people begin to assess out what is urgent and what is my anxiety, and how am I using my anxiety... how does my anxiety show up in ways that make me constantly want to produce, produce, produce, create, create, create, so that I don't have to be present with my own fears, my own frustrations. Are you using work as an escape mechanism, but having a negative impact on people in the workplace, right? And so, we see this happening a lot in a lot of spaces in a lot of organizations.
Yolo Akili Robinson (00:45:55):
I tell people to create water cooler time, time to share our non-work related things. This has been a really big thing that many of our clients have found helpful. We talk about building in an hour, maybe once or twice a week, where staff meet together and just be able to check in about what's going on in their lives. Whether it's their dog, whether it's what's going on with their kids, whether it's what's going on with what they're watching on television. Right now because we are all in this virtual space, many of us don't get the opportunity to really sit around the water cooler or the type of conversations that really help sustain and nurture us in our work. And so, it's really important that we build in time to just be, "Hey, what's going on with you? How are you? How are things happening?" Those pieces are really important.
Yolo Akili Robinson (00:46:38):
I'm going to say the slide... the next one... people might see it in kind of a... some people will hopefully see it in the [inaudible 00:46:45], realize the necessity of it. Stop forcing Black people and brown people into conversations about race with white people at work. I'm going to say it one more time. Stop forcing Black folks into conversations about race with white people at work. There is a tendency in the DNR world to create these spaces that create so much distress and duress for Black folks, where Black folks are forced to, often with superiors or people who are in the hierarchy above them, help hold and address racism, right? Help hold and address transphobia or misogyny.
Yolo Akili Robinson (00:47:21):
I really want to encourage people to really think critically about how... people they engage when they do these particular models. It is actually not helpful for many Black folk, I don't want to talk to you about race. Many women will be, I don't want to talk to you about the misogyny or sexism in this space because actually there are so many consequences for myself when I do that, that actually it creates more health challenges for me or more wellness challenges for me.
Yolo Akili Robinson (00:47:45):
So, thinking about creative ways, how do we educate white people about their racism without having Black people do that labor? How do we educate cis gendered people about their cis sexism without having trans folks do that labor? What does that look like, right? In this moment when so much murder of trans folks is happening, so much racism, so much increased police violence is happening, or our awareness of it at least, what are the things, what are the strategies we can do that do not put the burden on the people impacted to explain to the people who are not impacted about it?
Yolo Akili Robinson (00:48:14):
The last two pieces is wellness surveys. Really talking to people about what's going on in the office around race, gender, sexual orientation, and conflict challenges? What is the real culture? A lot of times when we talk about mental health we tend to externalize it, but really think about how is... what is the environment that we are cultivating in terms of for people to be able to express their feelings, be heard? What does that look like, right?
Yolo Akili Robinson (00:48:39):
And then the last one is emotionally intelligent leadership training, which really encompasses all of this and is a large part of what we do. Really holding space for us to begin to hold the nuances of all these pieces.
Yolo Akili Robinson (00:48:50):
One of the pieces that we talk about at BEAM, in our work, is we don't ask the question are you racist, sexist, or transphobic? We don't think that's a helpful question to ask. The question we think is more useful is, where is the racism, the sexism, the transphobia, the homophobia that you've learned all your life as a person living in this world showing up in your behaviors, ideas, and choices? So, we're not exempt, none of us.
Yolo Akili Robinson (00:49:12):
So, as a person myself, as a non-binary person, born in a body projected and read as male, I've received innumerable psychological and social benefits from the system of patriarchy that benefits men. It says that men and maleness are dominate and I have the right to rule. It says the characteristics that are masculine and male should be praised more than those characteristics associated with women and femininity, right? And because of that, whether I consider myself a good person or not, I have internalized ideas that show up in my behaviors and my treatment of other women in my space, right? And so the question is never, am I sexist, but where is the sexism showing up? And it's not about being a moral question, it's about the reality we all internalize these things.
Yolo Akili Robinson (00:49:52):
So, for white folks in the room who feel they are good people, the question is not about you being a good person or a bad person, it is about how is the racism and the ways in which you have internalized it unconsciously, and not so unconsciously, showing up in the ways in which your treating Black and brown folks, trans folks, queer folks in your space because we all learn messages that certain lives are less valuable. And whether we are conscious of them or not, they show up in the way we are in the world.
Yolo Akili Robinson (00:50:18):
I'm at my three-minute marker. I know I've said a lot. I just want to really briefly go over some quick pieces. We have some of the great tools on our website to help with conversations about these pieces. I want to invite you to visit at BEAM.COMMUNITY. It is not beam.com, it is BEAM.COMMUNITY. People often think to ask that. And some of these tools are really great tools to begin to think about how do you build up your capacity to really have conversations around the mental health and wellness in your space.
Yolo Akili Robinson (00:50:45):
Someone mentioned mental health first aid earlier, [inaudible 00:50:48] offer, that is a great program. However, one of the challenges of mental health first aid is [inaudible 00:50:52] of any kind of historical context, and it also focuses heavily on diagnoses as opposed to focusing on giving people skills. We do not believe that people who are not peer support workers, who are not clinicians, need to know the ins and outs of diagnosis. They need to understand some symptoms, and they need to have skills and strategies to show with folks, understand that it will be different in different communities, whether that's Black, LatinX, Asian Pacific Islander, or Native communities.
Yolo Akili Robinson (00:51:15):
And so, we have some tools here that you can learn more about on our website. We encourage you to visit and share. We also have a Black Virtual Wellness Directory which features a variety of Black wellness professionals who can help with supporting folks with Black Virtual Wellness care.
Yolo Akili Robinson (00:51:31):
So, that's three minutes, my time is up. You can learn more on our website, beam.community. You could sign up for our ListServe as well and find more about work there [inaudible 00:51:41].
Cait Ellis (00:51:43):
Great. Thank you so much, Yolo, for sharing your approach and model, and sharing those helpful and key steps to cultivate wellness in the workplace.
Cait Ellis (00:51:52):
We would like to use the remaining time to engage in a Q and A session with our audience. Please continue to submit your questions in the Q and A tab. At this time, I can ask all of our panelists to go ahead and come off mute. I will start by asking Brad a question, and I welcome the other panelists to jump in. We had a few questions come in related to telehealth.
Cait Ellis (00:52:14):
How has the move to telehealth... tele behavioral health impacted behavioral health equity for high need populations, and did you learn anything about limitations during this time of rapid deployment?
Brad Lerner (00:52:28):
Yeah, no, that's a great question. Well, absolutely it has shed the light early on on internet access. So, there was... telehealth is envisioned as a two-way audiovisual media. But in order to have that sort of visual component, you would need high speed internet, smart phones, and the like. And for communities that did not have that, that were poorer, more rural communities, we're going to see less opportunities to have those devices and that internet access.
Brad Lerner (00:53:03):
So, then you moved into sort of an audio component of treatment. That would be maybe doing psychotherapy or cognitive behavioral therapy over the telephone, the plain old telephone system. And there, you would have some concerns possibly. There's been less efficacy studies about certain types of treatment, higher levels of treatment and applied behavioral analysis. There just hasn't been widespread investigation about audio only sort of services for all treatment. Although, certainly having the continuity of care, as I mentioned earlier, was so important.
Brad Lerner (00:53:41):
So, I think going forward, health equity in terms of making sure folks will have access to the internet and to the devices to be able to access the telehealth will be a key market. And if not in communities, we'll have to look more at the efficacy of audio only.
Cait Ellis (00:54:04):
Thank you. Our next question was directed to Kathy, and I'll start with her and then we can open it up to our other speakers.
Cait Ellis (00:54:11):
How do we adapt for more mental and emotional resiliency as a group, and as individuals? And then, Kathy, can you also define shadow pandemic?
Kathleen Pike (00:54:23):
So, the shadow pandemic that has been referenced time and again is the idea that in the shadow of the infectious pandemic of coronavirus, the mental health symptoms will become so intense and widespread that they will be their own pandemic, landing in the shadow of the coronavirus pandemic. And on that point, to build on what Brad has said and what Yolo has said, the mental health needs are unquestionably real, but there are many strategies that can help all of us address our mental health needs in ways that can happen in community. And with the right community support, with the right organizational support, with the right leadership, so that we reduce the amount of really serious mental health consequences.
Kathleen Pike (00:55:25):
And some of those are going to look like mental health interventions, like mental health crusade, or training individuals in the community to recognize mental health symptoms, as Yolo described. But they also are not going to look like mental health interventions. They look like keeping people employed, they look like forgiving rental agreements, et cetera. So, that's the context of this shadow pandemic.
Kathleen Pike (00:56:01):
The other question was about building resilience. Cait, can you-
Cait Ellis (00:56:07):
Yes.
Kathleen Pike (00:56:08):
... say again?
Cait Ellis (00:56:08):
The question came in, yeah, looking at mental and emotional resiliency, both as an individual, but then also in a group setting.
Kathleen Pike (00:56:16):
So, one of the things that I think is really important right now, the image that is useful to me and I hope would be useful to others, is around gardening. That resilience, when you develop a garden, and you care and tend a garden, you take out weeds. And that is very much a clinical, medical model, so to speak, of taking out the things that you don't want. A symptom pull, right? But you'll never have the garden you want without planting what you hope to grow. And so, resilience strategies, resilience models are, poetically speaking, what garden do we want to grow? And so, what are we planting now to promote strength, to promote connection, to promote supports that enable people to engage with each other, remembering that all of this... keeping in mind what our goals are?
Kathleen Pike (00:57:21):
And I think to go back to Yolo's point, remembering that these are people, and that we work, our work is in the service of supporting the human structures, conditions, individuals, and communities, and we should make sure that we're doing just that and not the reverse.
Cait Ellis (00:57:46):
Great, thank you. So, we've had several questions come in around this idea of Zoom fatigue, whether it's individuals working virtually from home, or through telehealth, or even workers that are doing home visiting programs that are having to virtually connect with their patients. I'm wondering if anyone can talk to some concrete suggestions to really combat this Zoom fatigue that so many people are experiencing?
Yolo Akili Robinson (00:58:18):
Well, I would like to say something. I think the first piece we can do is consent. You would be surprised at how often many of the staff of organizations we're talking to, there is no kind of consent. If we're going to have a Zoom meeting, there's an expectation often that everyone has to be on camera and be visible. And what does it mean to give people the actual option to say, "I'm just going to call in, I don't feel like being visible today."
Yolo Akili Robinson (00:58:45):
So, really beginning with that piece. And we talk about within infrastructure, in terms of workplaces, just having those discussions and dialogues. And I think the one thing I was trying to say as well, in the earlier piece, is really understanding that... we've held some Zoom trainings and conversations that have been really powerful and beautiful. People have left them and felt like they were really enriching and nourishing because we were really focused on making human connection, right, and not just being so task oriented.
Yolo Akili Robinson (00:59:11):
I think building in intentional time in your workplace, as a manager, as a leader, where it's really building a relationship and connecting with someone, is really important. To have that as a part of the Zoom culture as well. So, I would just say, one, being really intentional with consent around that piece with your staff, really assessing and checking in because we found that a lot of our partners who often want this kind of compulsion, everybody has to be on camera, at often workplaces where there's very little... there's a lot of distrust, there's a lot of frustrations and challenges that this era has only brought to the rise, to the forefront. So, I think that really being intentional about understanding that Zooming is not using it as a micromanaging strategy is really critical for people to be kind of cultivating wellness in the workplace.
Yolo Akili Robinson (01:00:02):
And that you also still need to really address those core issues and those core dynamics by bringing in [inaudible 01:00:08] facilitators that [inaudible 01:00:10] enough skills to help really center and structure the space in a way that really does center healing and wellness.
Cait Ellis (01:00:16):
Great, thank you.
Kathleen Pike (01:00:18):
Cait, this is Kathy.
Cait Ellis (01:00:18):
Yes, go ahead.
Kathleen Pike (01:00:19):
I would just add to Yolo's... I love what Yolo said. And in a very concrete way, what we have done with a number of teams is reserve, once a week, for that team meeting the first 10 to 15 minutes of something that we share that is not task oriented, as Yolo said, but really is about who are the people on the phone. And can be from simple things like share one of the comfort foods that you have made during this pandemic, to tell us what you've got on your home screen and why you picked that picture. And it really is an incredibly simple, but incredibly powerful, way for people to remember that we're three dimensional and there's a lot going on in our lives. And to connect in more humane and caring ways.
Cait Ellis (01:01:15):
Thank you. Unfortunately, we are out of time today. We're just at the 2:00 o'clock Eastern time mark. I would like to thank our excellent panel of speakers and our audience for joining us today for this important discussion. Your feedback is important to us, so please take a moment to complete a brief survey which can be found on the bottom of your screen.
Cait Ellis (01:01:34):
I would also like to point out that we have additional resources available on our website, including some from our panelists, and our recent infographics on how the pandemic is impacting the mental health of employees, parents, and children.
Cait Ellis (01:01:47):
Thank you again for joining us today.
Presentations
Mental Health and Work: A Perennial Priority Peaks in the Wake of COVID-19

Kathleen Pike, PhD
Columbia University
More Related Content
See More on: Behavioral Health | Coronavirus